Every year, the average Australian takes over 2.7 million steps. That’s a lot of weight, pressure, heat and kilometres for our feet to cover – and often with little rest or breaks in between. With Valentine’s Day around the corner, we thought we’d swap out the notion of roses and chocolate with a thoughtful gift that will be very welcome by your partner or yourself – caring for your feet.
Here are five ways that your local My FootDr clinic can help care for and pamper your feet this Valentines Day – while doing your feet a world of good medically speaking to keep you going through all those steps.
1. Cosmetic Nail Restoration
Cosmetic nail restoration is loved by both men and women, and those that:
- Are unhappy with the look of their toenails
- Are battling a fungal nail infection
- Have trauma to their toenails from an injury or accident
- Have medical conditions like psoriasis that are changing the appearance of their nails
It’s also the perfect solution to improve the appearance of toenails in one appointment for those that don’t want to risk substandard safety and hygiene protocols, and hence infection risk, reported to be found in many traditional nail salons due to a lack of sterilising instruments between use on multiple people.
Using the KeryFlex proven nail restoration system, our experienced and board-registered podiatrists create a flexible, non-porous and realistic looking nail over your existing nail. It is durable and is unaffected by acetone, nail polishes or detergents – meaning you can paint it as you please! Aside from the immediate improvement in appearance, your natural nail will continue to grow out beneath the new nail.
Learn more about Keryflex here.
2. A Skin And Nail Care Appointment
Our skin and nail care appointments, often referred to as ‘general or clinical podiatry’, are comprehensive and all-inclusive appointments that immediately care for your nail and skin concerns, give your feet a fantastic tidy-up, and leave you feeling much more comfortable on your feet than when you first walked in.
With the majority of our patients having these appointments every 6-8 weeks to keep their feet feeling great and in tip-top shape year round, we welcome you to experience this foot care, completed by our experienced podiatrists, as a one-off treat, too. Your podiatrist will take care of any lumps, bumps and even the thickest or curliest of toenails. This includes:
- Immediate and pain free removal of corns on toes and feet
- Conservative care for ingrown toenails (non-surgical)
- Reducing thick, cracked heels
- Removing or reducing thick and uncomfortable patches of callused skin
- Trimming toenails, no matter how thick or stubborn
- Clearing the sides of the nails from debris and hard skin build-up
- Starting to care for plantar warts
We love these appointments due to the immediate relief patients feel when they put their feet down on the floor after this care – which is often the difference between feeling like they’re constantly walking on a pebble (of hard skin beneath their feet) and feeling like they’re walking on air.
3. Care For Cracked, Painful Heels
While some people get away with minor cracks that can be cared for in a skin & nail care appointment (above), after a long summer and many months of wearing thongs – which many still wear daily – cracked heels are a big problem around this time, that we see and treat very effectively with these specific appointments.
As cracked heels start with hard, dry skin that thickens and worsens over time, our podiatrists work to remove all the excess dead skin – a process that is usually simple and painless using our sterile instrument range. We ensure that no sharp edges are left that will catch on your carpet or socks, which could otherwise pull the skin, creating significant damage.
Treating cracked heels now, and not at the end of the summer, is a great preventative measure to stop cracks progressing deep down into the healthy, supple skin beneath. We call this the danger zone, as deep cracks in this area can quickly leave you vulnerable to infection by creating portals of entry for bacteria, fungus, viruses – and a great deal of pain – that you often can’t reach on your own.
4. Comfortable Footwear
Our shoes become the ground we walk on and determine what and how our feet feel. That’s why if you choose your ground to be a hard plastic, the chances of your feet feeling tired and achy, or the chance of you developing foot pain, is much higher.
This is exactly why so many of our clinics offer a footwear range so you can try on and get the best shoes for your feet – and not just that feel great, but fit your foot type, too. We have podiatrists and trained staff available to ensure you get the best fit and maximum comfort.
Don’t have a My FootDr near you? That’s okay! We have an online store too.
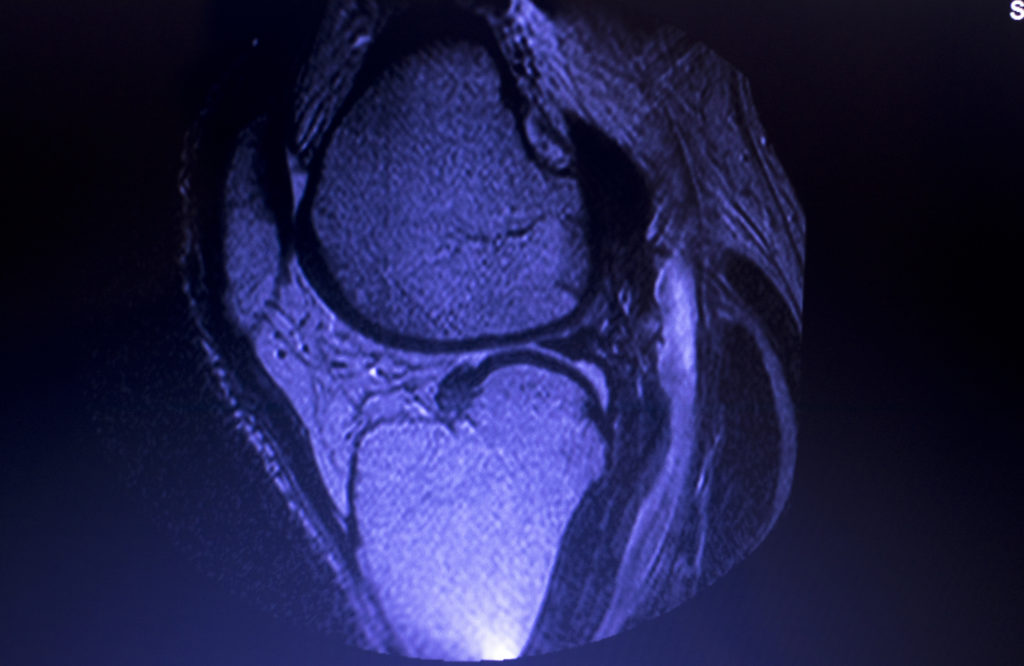
5. Treating Those Lingering Aches Or Pains
Finally, the best way we can think of to treat your feet this Valentine’s Day – or help your loved ones treat theirs – is to care for those lingering aches, pains or injuries. You know, the ones you may be hoping will get better on their own, or that you know you need to have seen, but it’s been a crazy last 12 months (which it absolutely has!).
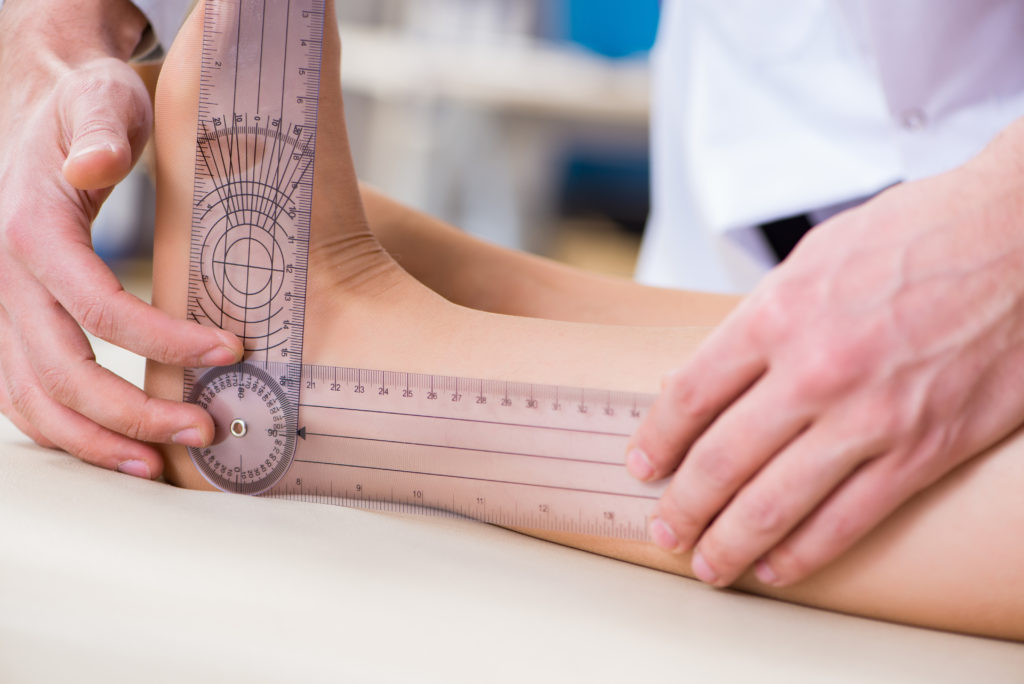
This is done through a biomechanical appointment, where our experienced podiatrists look at:
- Which tissues, muscles, ligaments or structures are causing your discomfort or pain
- The strength and flexibility of the involved joints and muscles
- Your foot posture
- Comprehensive analysis of your gait (the way you walk) and how your feet and legs engage during walking and/or running
- Pressure testing of both feet
Alongside your history and a series of other questions, this consultation will determine the how, what and why of what’s going on – followed by an optimal plan to get you pain-free and feeling great!
Ready To Feel Great On Your Feet?
Our podiatry team are ready when you are! As the largest podiatry provider in Australia, we’re proud to be your trusted local podiatry providers, committed to delivering exceptional service, every time. Book your appointment with us online here or call us on 1800 FOOT DR.