
Do itchy feet keep you awake at night?

The medical term for itchy feet is pruritus, and this regular or recurrent itch can feel extremely frustrating for those affected. While the science behind why we itch in the first place isn’t well understood, it is thought to be a way to protect the skin from parasites, dead skin build-ups, and any other nasties that are wanting to move through the skin and invade our bodies where they can do real harm. Which makes sense! When a mozzie or other bug starts biting, you feel an itch, look down, see the bug there and shoo it away before it does too much harm. It also explains why when you see someone else itching, you may itch too – to help prevent whatever is biting or irritating the other person to get to you too.
While this is great protection, it doesn’t make the sensation any less unpleasant and downright maddening at times. If you’ve found yourself regularly itching your feet or your toes and have no idea why, our podiatry team have put together the top six reasons that your soles, toes or feet, in general, are itchy – and what you can do to help stop the itch.
1. Dry Skin On The Feet
Dry skin is irritated skin. If the natural oils on your feet dry up or stop doing their job to moisturise and care for the skin, the skin gets irritated, starts getting that dry and flaky appearance, and starts to itch.
The solution is to fix the dryness. This is easiest done by giving the feet a good wash and scrub to remove the dry, dead skin and applying a good moisturising lotion daily to replace the function of the natural oils. If your feet are covered in callus or hard cracks, we can take care of all of this for you at a skin & nail care appointment.
2. Athlete’s Foot Fungal Skin Infection
 Medically known as tinea pedis, Athlete’s Foot is a common skin infection that tends to affect the soles of the feet and between the toes. It can make the skin look dry and powdery, have bubbles that look like they’re peeling and may look red and irritated. These changes to the skin, as well as the presence of the fungus, can cause the skin to get very itchy.
Medically known as tinea pedis, Athlete’s Foot is a common skin infection that tends to affect the soles of the feet and between the toes. It can make the skin look dry and powdery, have bubbles that look like they’re peeling and may look red and irritated. These changes to the skin, as well as the presence of the fungus, can cause the skin to get very itchy.
The solution is to use an anti-fungal medication to treat the fungus, and help prevent the fungus from returning by helping keep your feet dry as much as possible, like proactively drying your feet well after showers – especially between the toes. This is because fungus grows best in moist, warm environments – like damp socks and shoes.
Learn more about Athlete’s foot here.
3. Nerve Damage
Much like experiencing burning, tingling, pins and needles, nerve damage can also cause other abnormal sensations which can include itching. When it comes to the feet, diabetes is a large cause of nerve damage that we work with, while other causes of a neuropathic itch reported in studies include shingles and neural lesions, among others.
The solution: unfortunately, these itches are tricky to treat and manage as the nerve damage is often irreversible. Some medications have been reported to help, so seeing your GP or your My FootDr Podiatrist for a definitive assessment is your first step.
4. Chilblains
Chilblains develop when the blood vessels in your feet change from being constricted (narrowed) due to the cold temperatures, to dilating quickly when they warm up and sending blood streaming through the vessels. The result is that blood can leak into the surrounding tissues, and may become very itchy very quickly. You must be super careful, as your skin can be more vulnerable to damage when you have chilblains, making scratching particularly damaging
The solution is prevention. Chilblains are preventable by avoiding going from cold to hot too quickly. Instead of jumping straight into a hot shower or bath with freezing feet, let them defrost and adjust to room temperature first, wear some socks to help them warm up gradually, and avoid applying direct heat in the form of a heat pack or putting your feet up next to an open flame.
5. Medical Conditions & Medications
 Both medical conditions and medications can also cause itchy feet. When it comes to medications, common ones you may already be taking include aspirin, some pain killers (opioids) and some blood pressure medication can get the skin itching.
Both medical conditions and medications can also cause itchy feet. When it comes to medications, common ones you may already be taking include aspirin, some pain killers (opioids) and some blood pressure medication can get the skin itching.
When it comes to medical conditions, this can range from kidney, liver or blood problems, to having an overactive thyroid, to skin conditions like chickenpox, psoriasis, eczema, hand-foot-and-mouth disease and more.
The solution lies in addressing the cause – whether that’s managing the condition, or altering your medication with your GP to help avoid this symptom.
6. Allergies & Contact Dermatitis
If your skin appears to have a reddened, rash-like appearance that may have some blistering and has some significant itching, then it may be an allergic reaction or contact with an irritant that may have triggered contact dermatitis. Contact dermatitis simply means inflammation and irritation of the skin (dermis), and can present on the feet unexpectedly as a result of glues or chemicals found in shoes, contact with irritants found in nature when walking with bare feet, or even skin and nail care products.
The solution is to identify and remove the allergen or irritant that has triggered the problem, and hence the itching. In the meantime, the itching sensation can be relieved using creams and corticosteroids from your chemist or GP.
Scratching: The Consequences And Why It Feels So Good
While scratching your feet when they itch is the normal – and often uncontrollable – response to give you some much-needed temporary relief, it can also make the problem worse by irritating or even damaging your skin, leaving you with some discomfort or being vulnerable to infection. So as much as possible, try to avoid itching!
For your interest, scratching can feel so good because it sends a low-level pain signal to your brain that overrides the itching sensation, providing relief. Unfortunately, it can also trigger a cycle that re-activates the itch signal, leaving you in a constant state of itching and scratching.
Itching for help?
If you’re worried about your feet, we’re here to help. My FootDr has clinics all around Australia with knowledgeable, experienced podiatrists to help you get the best results for your feet. Book your appointment online or call us on 1800 FOOT DR

 If you have flat feet, knowing which insoles are right for your feet can be difficult and confusing. There are so many types out there, which may leave you with a lot more questions than answers, like:
If you have flat feet, knowing which insoles are right for your feet can be difficult and confusing. There are so many types out there, which may leave you with a lot more questions than answers, like: 


 Every week, almost half of all Australians experience foot pain. As foot health experts here at My FootDr, this comes as no surprise – our feet support the entire weight of our bodies, and with hundreds of moving parts, the role of our feet is more complex than many of us realise. With our feet being a small but mighty collection of muscles, tendons, ligaments, bones and nerves – when something is overloaded, out of place or not functioning quite right, it can be an easy road to foot pain.
Every week, almost half of all Australians experience foot pain. As foot health experts here at My FootDr, this comes as no surprise – our feet support the entire weight of our bodies, and with hundreds of moving parts, the role of our feet is more complex than many of us realise. With our feet being a small but mighty collection of muscles, tendons, ligaments, bones and nerves – when something is overloaded, out of place or not functioning quite right, it can be an easy road to foot pain. 
 Do you have private health insurance? With a large number of private health funds having a deadline of
Do you have private health insurance? With a large number of private health funds having a deadline of 

 Medically known as
Medically known as  Both medical conditions and medications can also cause itchy feet. When it comes to medications, common ones you may already be taking include aspirin, some pain killers (opioids) and some blood pressure medication can get the skin itching.
Both medical conditions and medications can also cause itchy feet. When it comes to medications, common ones you may already be taking include aspirin, some pain killers (opioids) and some blood pressure medication can get the skin itching.
 If you hold a DVA gold card, you may be eligible for a number of
If you hold a DVA gold card, you may be eligible for a number of 
 It’s Australian Tradies National Health Month and to help support tradie health and encourage a healthy workplace through injury prevention management, our podiatrists are talking about your
It’s Australian Tradies National Health Month and to help support tradie health and encourage a healthy workplace through injury prevention management, our podiatrists are talking about your 
 Tradies – you feel
Tradies – you feel 
 Here at My FootDr, we have the privilege of helping men and women with a wide range of lower limb problems. This gives us a unique insight into the kinds of injuries men and women tend to sustain more frequently, and the causes behind them. We believe that knowledge is power – and that knowing your risks is a powerful tool to help avoid painful and potentially long-standing injuries. So today, we thought we’d pair our observations with the current research to help answer an all-too-common question:
Here at My FootDr, we have the privilege of helping men and women with a wide range of lower limb problems. This gives us a unique insight into the kinds of injuries men and women tend to sustain more frequently, and the causes behind them. We believe that knowledge is power – and that knowing your risks is a powerful tool to help avoid painful and potentially long-standing injuries. So today, we thought we’d pair our observations with the current research to help answer an all-too-common question: 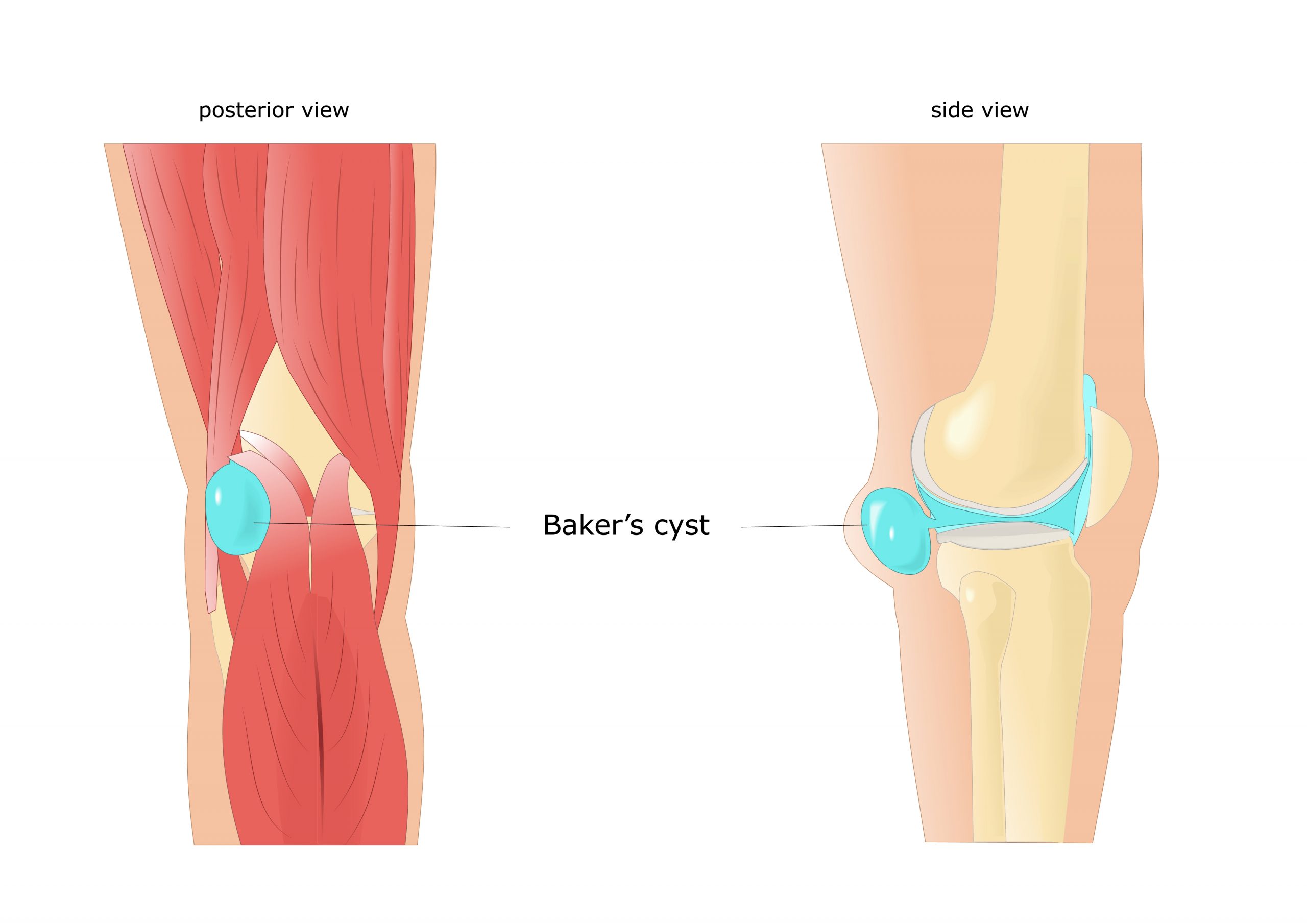
![AdobeStock_89895636-bakers Cyst [Converted]-01](/wp-content/uploads/AdobeStock_89895636-bakers-Cyst-Converted-01-300x212.jpg) Recently, we treated a social runner in his 50’s who was experiencing pain and swelling behind his knee. He couldn’t recall any injury or reason for the pain, but it seemed to be getting worse, especially when he bent or straightened his knee. With a careful examination, history taking, medical imaging and consultation with his GP, he was diagnosed with a
Recently, we treated a social runner in his 50’s who was experiencing pain and swelling behind his knee. He couldn’t recall any injury or reason for the pain, but it seemed to be getting worse, especially when he bent or straightened his knee. With a careful examination, history taking, medical imaging and consultation with his GP, he was diagnosed with a  As a My FootDr podiatrist, the phrase “I get [insert body part] pain during or after running” is something we hear
As a My FootDr podiatrist, the phrase “I get [insert body part] pain during or after running” is something we hear